As a care provider, you’ll probably need to manage challenging behaviour during your career.
You might support clients with severe learning disabilities, people with dementia, or autistic people. Many people who struggle to communicate will display challenging behaviour. They might hurt others or themselves, destroy property, attempt to run away, or scream.
It can be hard to know how to react to these actions, but all care workers should be confident in managing challenging behaviour.
In this guide, we’re looking at strategies for dealing with challenging behaviour in adults. However, many of these techniques are also useful if you work with younger people and are managing challenging behaviour in children.

Table of Contents
What is challenging behaviour in care?
Challenging behaviour in care is the term for a range of actions that can put a client or those around them at risk, or give them a poorer quality of life.
Challenging behaviour might include:
- Aggressive behaviours, such as biting, hitting, or kicking
- Self-injury, like head banging, scratching, or hand biting
- Disruptive behaviours, like running away, shouting, or removing clothes
- Eating inedible objects
- Destroying property
You might also hear challenging behaviour called behaviour that challenges, erratic behaviour or disruptive behaviour. Many people prefer the terms behaviour that challenges or challenging behaviour, because they focus on how people and services respond to the actions, rather than criticising the client.
Who shows challenging behaviour?
Anyone can display challenging behaviour. However, in care, the term usually refers to behaviours shown by people who can’t communicate their needs – such as autistic people, people with advanced dementia, and those with severe learning disabilities.

What is the cycle of challenging behaviour?
There are several phases to challenging behaviour; it doesn’t usually come out of nowhere.
The cycle of challenging behaviour has four phases:
- Trigger: This is what sets off the cycle. A trigger could be pain, a loud noise, or being asked to stop a favourite activity. Carers should learn to recognise a client’s triggers, and minimise them if possible.
- Escalation: The client becomes more distressed. During this phase, carers and others may be able to prevent the cycle from progressing further – for example, they could try distracting the client, speaking calmly, or moving them away from the trigger.
- Crisis: The client is highly distressed, angry, or upset, and displays challenging behaviour. Carers should act to make sure that clients and others are safe.
- De-escalation and recovery: The immediate crisis is over, although the client may still be upset. They may also be tired, or easily triggered again. Carers should learn what helps each client after a crisis.
What is Positive Behaviour Support (PBS) in care?
Your organisation might use PBS strategies to support clients. PBS, or Positive Behaviour Support, is a person-centred approach to helping clients who display challenging behaviours. It aims to stop the cycle of challenging behaviour before it starts.
As a care provider using PBS, you’ll work to understand the reasons behind their behaviour, and attempt to use proactive strategies to keep them feeling calm and relaxed.
You might do this by making changes to their environment or routine to minimise triggers, and by looking out for the early warning signs of distress.
Book a free tour
Looking for calmer, more consistent care?
See how PASS helps care teams plan support, record incidents clearly, and keep everyone aligned when managing challenging behaviour.
From structured care plans and risk management to shared notes and clear oversight, PASS supports safer, more confident care every day.
How to deal with challenging behaviour
When your client is displaying challenging behaviour, it can be difficult to know how to react.
It’s important to remain calm and make sure that your client stays safe. You should document challenging behaviour and look for triggers, and keep communicating with colleagues and family members.
9 ways to manage challenging behaviour:
- Stay calm
- Make sure your client and others are safe
- Listen to your client
- Document everything
- Communicate with family members
- Communicate with colleagues
- Involve other healthcare professionals
- Look for training in managing challenging behaviour
- Ask for further help
We’ll provide some strategies for dealing with challenging behaviour in adults here. For care managers, we’ll also offer some advice on how to support your staff team when they’re helping clients who display challenging behaviour.
Stay calm
Challenging behaviour can often be very frustrating for care workers, and it can be hard to stay calm – especially if a client is being violent towards you or making hurtful comments.
However, it’s important to avoid getting upset or angry.
Remind yourself that your client’s actions aren’t personal. Your client is distressed and doesn’t have another way of expressing their feelings.
How care managers can help their staff team stay calm:
- Check in with your care team regularly, especially if they’re supporting clients who display challenging behaviour.
- If possible, increase the length of care visits, so that your carers don’t need to rush.
- For clients who display especially challenging behaviour, consider scheduling two carers – this gives each person time to step away if necessary.

Make sure your client and others are safe
Many challenging behaviours can put clients and others at risk. Your priority is to make sure that everyone is safe from harm.
Depending on the situation, this might mean removing your client from the room, or asking others to leave. You might need to take dangerous objects away from your client, distract them, or, in certain cases, restrain them.
How care managers can help to ensure everyone is safe:
- If necessary, schedule two or more carers to support a client.
- Avoid leaving a single care worker alone with a group of clients.
- Make sure your care workers understand your organisation’s policies around restraint.
Listen to your client
When a client displays challenging behaviour, remember that it’s often a symptom of something else.
Clients may struggle to communicate their feelings through words or signs, but behaviour is communication.
Sometimes, it’s clear what your client is trying to communicate. Maybe they consistently display challenging behaviour when offered a certain meal – this could indicate that they don’t like this food.
However, identifying the causes of challenging behaviour isn’t always that easy. You can use ABC behaviour charts to document your client’s behaviour and the situation that led up to it. This can help you work out triggers.
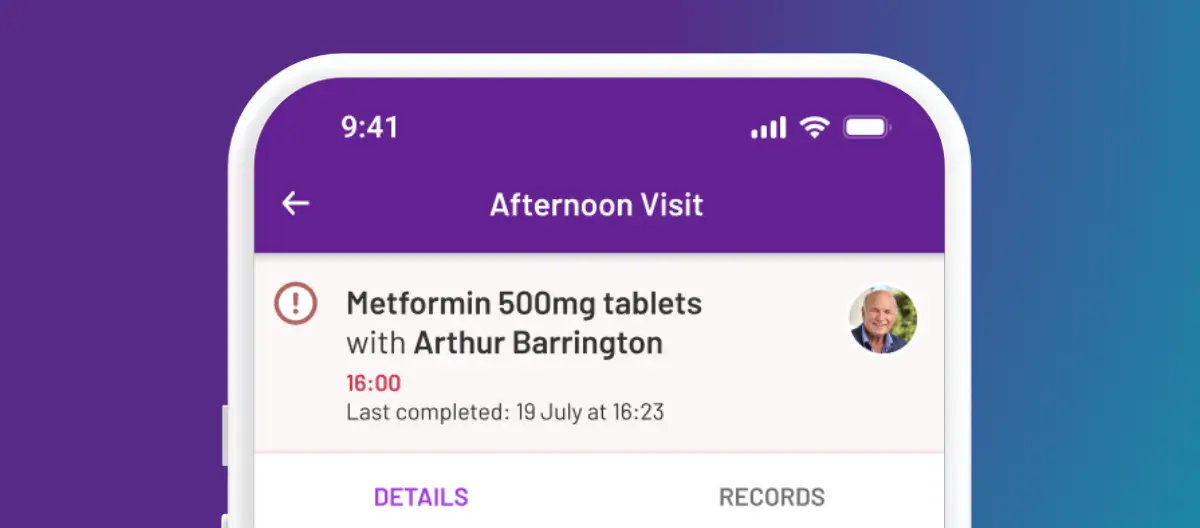
During the care planning process, talk to your client and their family to build a comprehensive picture of their needs and preferences. Capture everything, from hated foods to favourite clothing. Care planning software, like PASS, can help you record this information and share it with the entire care team.
How care managers can help their staff team listen to clients:
- In your initial care planning meetings, gather as much information as possible about the client’s needs and preferences. Make sure these are recorded somewhere that care staff can easily access.
- Make sure that care visits are long enough for carers to spend time with clients and get to know them.
- Encourage your care team to use ABC charts and document potential triggers.
Document everything
Documenting challenging behaviour can help you identify triggers. However, it’s also important for other reasons, including:
- Accountability: Documenting incidents accurately can help protect you from accusations of abuse, especially if your client self-harms and has visible injuries.
- Noticing an increase in frequency or severity of incidents: Accurate documentation can help you see if your client is displaying challenging behaviour more often, or if the incidents are more severe than in the past.
- Providing evidence to other health or social care professionals: If you need to ask for funding for more care hours, suggest a client moves to a more suitable care facility, or request further support from their healthcare team, accurate notes can be helpful.
Care management software, like PASS, can help you document challenging behaviour. Here’s how care managers can help their staff team document everything:
- Make sure that your team has access to care management software, if possible.
- Regularly audit your team’s notes, so that you can pick up any issues quickly.
Communicate with family members
If it’s appropriate, talk to your client’s family and friends about their behaviours.
Relatives and friends might have more insight into the reasons behind their actions, or have suggestions about how best to support them.
How care managers can facilitate communication with family members:
- Encourage your staff team to talk to family members when they see them, and document these conversations if necessary.
- Use care management software, like PASS, that lets you easily communicate with family members.
- Arrange regular meetings with family members to review the client’s care.

Check in with colleagues
If other colleagues also support your client, talk to them. They may have noticed triggers that you’ve missed, or have their own techniques for supporting them through their challenging behaviour.
Working together, you may be able to understand your client more and help them stay calm.
If you’re new to supporting a particular client, it’s especially important to ask for support from your colleagues. Other care workers might have known the client for longer, and know how to keep them calm, or how to support them when they are feeling particularly anxious or unhappy.
Talking to colleagues might be easy if you work in a care home or other residential facility. You probably have regular handover sessions, and you might even work the same shifts.
However, if you provide domiciliary care for a client, it can be difficult to find the time to talk to your fellow care workers. Home care software like PASS can help you here.
You can use the app to communicate with colleagues, and record any incidents that happen during care visits, so that everyone who supports a client can see what happened and learn from it.
How care managers can help their staff team work together:
- If your working arrangements permit it, arrange standup handover sessions at the start and end of every shift, so carers can share updates.
- If your staff team don’t regularly see each other, make sure they have a way to communicate – this could be through care software, a secure messaging app, or a work email system.
- Arrange regular team socials, so colleagues can get to know each other outside of work.
Involve other healthcare professionals
Your client’s behaviours might be exacerbated by pain, nausea, constipation, or other conditions.
Where appropriate, you may need to talk to other members of your client’s healthcare team about their behaviour.
If your client’s behaviour has suddenly changed, talk to their healthcare team immediately.
Sudden aggression or confusion can be signs of conditions that can become serious if left untreated – your client might have a urinary tract infection, or have sudden, severe pain.
How care managers can facilitate communication with healthcare professionals:
- Be willing to be the point of contact between your care team and other healthcare professionals.
- Use GP Connect to easily collaborate with your client’s GP and access their healthcare information.
Consider challenging behaviour training
Some organisations arrange challenging behaviour training as part of their standard training programme.
However, if your organisation doesn’t, or you’re a self-employed carer, you may need to find challenging behaviour training yourself.
The Challenging Behaviour Foundation runs workshops for family members and professionals. Alternatively, you could look for training through the National Autistic Society, the Alzheimer’s Society, or other organisations. You may want to take courses in strategies like Positive Behaviour Support, or find workshops about reducing the use of restraint when dealing with behaviours that challenge.
How care managers can help carers who want further training:
- Be proactive: look at your clients’ needs, and arrange appropriate training courses without your staff team requesting them.
- Pay for additional training courses if possible, or help your team to find funding.
- Hold regular development reviews for each member of staff. Ask if there are any areas where they would like further training.

Ask for further help
Sometimes you can’t support your client safely. If they continue to be a risk to themselves and others, you may need to ask for further help.
If you work for a care agency or in a residential facility, you could ask your care co-ordinator to put two carers on the roster for each care visit. If you’re employed directly by your client and their family, talk to them about your concerns.
In some cases, you may need to consider whether your care service is the best solution for your client. For example, if you work in a supported living facility and your client has advanced dementia, a specialist dementia care home might be more able to support them and manage their challenging behaviour.
How care managers can support their team to ask for help:
- Understand that asking for help can be daunting. Make sure that your team know it’s okay to need support.
- Make yourself available to your staff team, and ensure they know how to contact you in an emergency.
- If your organisation can’t support individuals with a high level of need, make sure that your staff team know this. Make your policies and procedures easily accessible to your staff team.
- Carry out regular care assessments, so that you’re aware of any clients who may need more specialist care.
- Be prepared to have difficult conversations with clients and their families. Considering a move to a specialist unit can be a very emotional subject, and you should be the one to lead this discussion, rather than individual care workers.
Closing words: Strategies for dealing with challenging behaviour in adults
When an individual displays challenging behaviours, it’s usually a sign of distress. They’re trying to communicate.
Managing challenging behaviour can be hard. However, it’s not something you should manage alone. Work with your colleagues, your client’s family, and other healthcare professionals to support your client.
Book a free tour
Supporting your team when care gets complex
See how the PASS care management platform helps you bring structure, clarity, and confidence to the moments that matter most.