In the world of health and social care, the focus is fundamentally moving from just treating health conditions to understanding and caring for people as individuals. This approach, known as person-centred care, is changing how care providers deliver care in the community.
This article aims to break down what person-centred care really means, how it works, and why it’s important for everyone involved in health and social care.
Whether you’re a care provider, a family caregiver, or even a receiver of care, understanding this approach is key to improving the quality of care and making the health and social care system better for everyone.
So, what exactly is person-centred care and why is it important? Let’s dive in together and find out.

Table of Contents
What is person-centred care?
Person-centred care is like putting the care receiver in the driver’s seat of their own healthcare journey.
Imagine a car. In traditional healthcare, the caregiver is the driver, and the care receiver is a passenger. The caregiver decides the route, the speed, and the stops along the way.
But in person-centred care, the roles switch. The care receiver becomes the driver, and the healthcare providers are the co-pilots, helping to navigate but not taking over the wheel. This involves:

Going beyond medical needs
A person-centred approach goes far beyond just meeting and fulfilling medical needs. It looks at the whole person. What are their emotional needs? What lifestyle do they live? What are their goals and priorities? All of this information helps to tailor a care plan that suits them best.
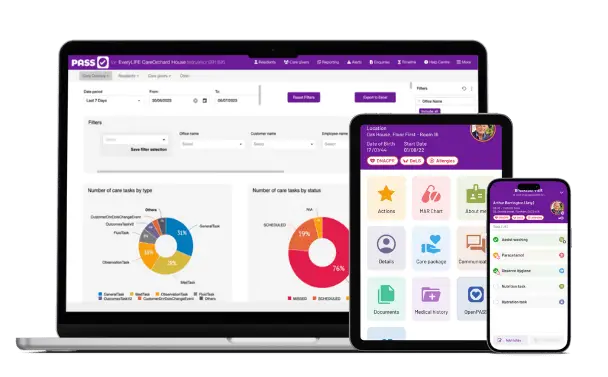
PASS care planning software, for example, features an ‘About Me’ page, on which a care receiver’s hobbies, interests, and preferences can be recorded, in line with the PRSB’s recommended best practice.
Read more: The Professional Record Standards Body (PRSB) ‘About Me’ Standard
Involving the individual
In this approach, health and social care providers work together with the care receiver.
They ask questions like, “How can we best care for you and achieve outcomes aligned to living well?” or “How can we make this care plan work for your lifestyle?”
By doing so, the person receiving the care feels heard and valued, which is crucial for any successful care plan delivery.
A team effort
It’s not just about the care receiver and care giver. The multi-disciplinary team (MDT), family members, and sometimes even friends are part of the care delivery team. Each individual contributes different insights to help to make the care plan more effective.
Flexibility is Key
Person-centred care is flexible. As the person’s needs and circumstances change, so does the care plan. That’s crucial because life is unpredictable, and health and social care needs to be able to adapt.
Section summary
Personalised care and support is a smarter and more respectful way of taking care of people. It’s about acknowledging that each person is unique and has different needs, preferences, and goals.
By adopting this approach, health and social care providers can offer better care, and care receivers are more likely to be engaged and satisfied.
What are the four key principles of person-centred care?
Now that we’ve established what a person-centred approach involves, let’s talk about the backbone of this approach – the key principles. These principles – defined by the Health Foundation – aren’t just abstract ideas; they’re actionable guidelines that help healthcare providers put person-centred care into practice.
Principle 1: Respect, compassion, and dignity
What it means
This is the cornerstone. It’s about treating the person in care as an individual deserving of respect, just like anyone else. This means listening carefully to them, respecting their wishes, and acknowledging their opinions.
In action
Let’s say you’re a health and social care provider. When you enter a care receiver’s living environment, instead of rushing through a checklist of questions, you sit down and engage in a conversation. You ask them about their day, their feelings, and their thoughts on their care plan. This level of interaction fosters dignity and respect.
Principle 2: Collaboration and coordination
What it means
This is about teamwork. Health and social care isn’t a solo activity; it involves cooperation between the care receiver, family, and professional healthcare providers.
In action
Take a family meeting as an example. Here, the multi-disciplinary team (MDT), the care receiver, and family members come together to discuss the care plan and treatment options, share insights, and make collective decisions. Everyone has a seat at the table, and everyone’s voice is heard.

Principle 3: Personalised care and support
What it means: Personalised care is about tailoring the care plan to the unique needs and preferences of the individual. No two people are the same, so their care plan shouldn’t be either.
In action: Consider the case of an elderly individual with multiple chronic conditions. The care team doesn’t just prescribe a standard course of treatment; they consult with the individual, family members, and multiple healthcare providers like the GP, nutritionist, and physiotherapist.
Together, they design a care plan that accounts for the individual’s specific health needs, lifestyle, and preferences. This could include medication schedules, dietary plans, and even hobbies or interests that contribute to overall well-being.
Principle 4: Participation in care
What it means
Participation is about empowering the individual to be an active part of their care. It means giving them the tools and information they need to make educated decisions.
In action
Let’s say a care receiver needs to decide between two different treatments. Instead of making the decision for them, the healthcare provider lays out the pros and cons and guides the individual to the option that aligns best with their values and lifestyle.
Section summary
By embracing these four principles, healthcare providers can ensure they’re delivering the highest standard of care that’s both effective and compassionate.
These principles make the healthcare journey a collaborative and empowering experience for everyone involved.
Examples of person-centred care
Understanding the theory behind personalised care and support is one thing, but how does it really work? Let’s explore some fictional examples to bring these concepts to life.
Example 1: Mary's customised care plan
Situation: Mary is an 80-year-old woman with Alzheimer’s. Traditional care models often focus solely on managing her cognitive decline.
Person-centred approach: After discussions with Mary and her family, the care team learned that she loves gardening and music from the 1950s. Her care plan now includes garden therapy and listening to her favourite Elvis songs, which not only lifts her spirits but also helps with her cognitive function.


Example 2: Ammar's active participation
Situation: Ammar, a 40-year-old with diabetes, is struggling with weight management and maintaining his insulin levels.
Person-centred approach: Instead of merely prescribing medication and dietary changes, Ammar’s healthcare providers involve him in setting achievable fitness goals. He chooses swimming as his preferred exercise and now attends a community pool twice a week. This involvement gives him a sense of control and accomplishment, enhancing his commitment to his health journey.
Example 3: Sarah's family collaboration
Situation: Sarah is a teenager who has recently been diagnosed with anxiety and depression. Typical care usually involves medication and perhaps some therapy sessions.
Person-centred approach: Sarah’s care team makes it a point to include her and her family in her mental health discussions. They come up with a strategy that mixes medication, counselling, and family support sessions. Sarah also opts to include art therapy as a form of expression, adding a unique touch to her treatment plan.
Read more: how PASS care management software empowers person-centred care

Why is person-centred care important?
We’ve talked about what person-centred care is and the principles that guide it. But let’s get to the heart of the matter: Why is this approach so crucial in healthcare? Well, here are some compelling reasons:
Improved care receiver experience
What it means
When health and social care is tailor-made to fit the individual, it’s no surprise that care receivers feel more satisfied and happier with their care. They feel heard, respected, and involved—basically, they feel like humans, not just case numbers.
Why it matters
Happy care receivers are more likely to be engaged in their own healthcare and follow medical advice. It’s a win-win for both care receivers and healthcare providers.
Better health outcomes
What it means
When a care receiver is actively involved and their unique needs are considered, treatment plans tend to be more effective.
Why it matters
Better treatment plans mean better health outcomes. That could be faster recovery from surgery, better management of chronic conditions, or improved mental health. Essentially, people may get better, quicker.

Increased efficiency and cost-effectiveness
What it Means
Believe it or not, personalised care plans can actually save time and money in the long run. The Health Foundation, for instance, found that when people are better informed they are less likely to use emergency hospital services and are more likely to stick to their treatment plan and take their medicines correctly.
Why it matters
When care plans are tailored to the individual, there’s less trial and error. This saves time for healthcare providers and often leads to fewer repeat visits for the care receiver. In the grand scheme, this efficiency can translate into cost savings for the healthcare system.
Strengthened care relationships
What it means
This approach fosters better communication and trust between care receivers and healthcare providers.
Why it matters
When there’s a strong relationship, care receivers feel more comfortable sharing their concerns and questions, leading to a more comprehensive understanding of their condition. This is crucial for effective treatment and long-term healthcare planning.

Holistic well-being
What it means
A personalised care plan takes into account not just physical health, but also emotional and mental well-being.
Why it matters
Health isn’t just about treating a symptom or a disease. It’s about overall well-being, which includes mental and emotional health. By adopting a person-centred approach, healthcare providers can offer a more complete form of care that benefits the individual in multiple ways.
Section summary
Person-centred care is more than just a nice-to-have; it’s a must-have in modern healthcare. It provides tangible benefits that elevate the quality of care, improve health outcomes, and even streamline costs.
And at its core, it brings humanity back into healthcare, making the journey better for everyone involved.
Key takeaways
- Person-centred care: It’s about putting the care receiver in the driver’s seat, focusing on their individual needs, values, and goals.
- Four principles: Respect and dignity, collaboration, participation, and personalisation are the backbone of this approach.
- Improved experience: Care receivers are happier and more engaged, leading to a win-win situation for everyone involved.
- Better health outcomes: Tailored care plans mean more effective treatments and potentially faster recoveries.
- Cost-effective: This approach can save both time and resources in the long run, benefiting the healthcare system.
- Strengthens relationships: Better communication and trust are built between healthcare providers and care receivers.
- Holistic well-being: It’s not just about physical health but also emotional and mental wellbeing.
How we can help
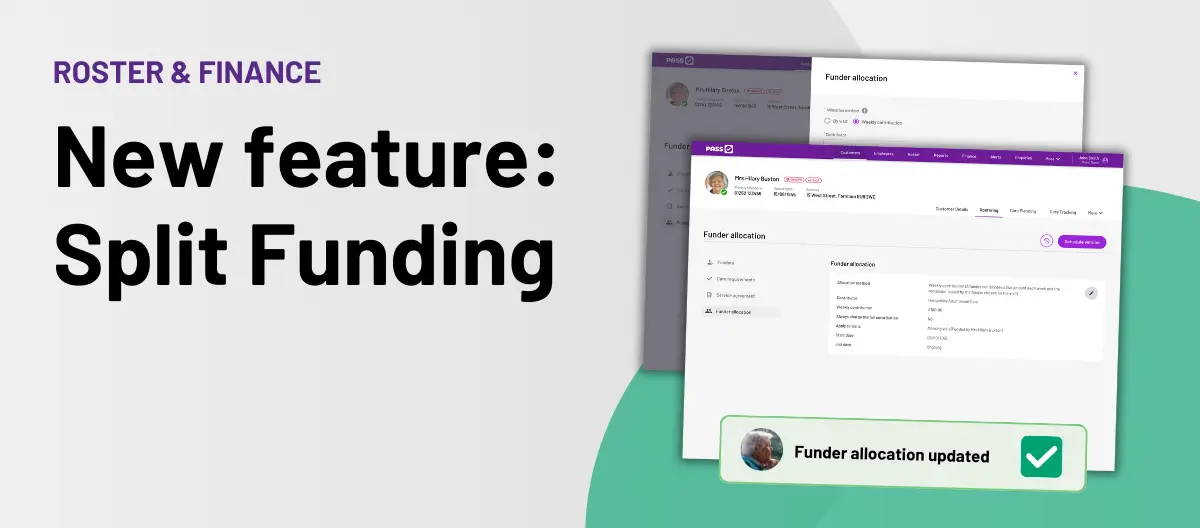
Discover how PASS Care Management Software can help your care service with features that support individualised care plans, transparent information sharing, and much more. Take the next step in transforming your care delivery. Get started with PASS today!
Disclaimer
The information provided in this blog is intended for general informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your healthcare provider or other qualified health professional with any questions or concerns you may have regarding your health or a medical condition.