A positive behaviour support plan can help you care for a client who displays challenging behaviours.
If you support clients who hurt others, self-injure, or are destructive, you probably want to encourage more positive behaviour instead. Many of your service users will struggle to talk about their feelings, and this challenging behaviour is usually a sign of distress.
As a care provider, you will need to recognise when your clients are using challenging behaviour to communicate. Part of your role will involve trying to understand the reasons behind a service user’s behaviour, and identify their needs.
Whether you use care management software to record behaviour or rely on paper records, having a consistent approach makes it easier to spot patterns.
In this guide, we’ll look in more detail at positive behaviour support, who can write a positive behaviour support plan, and some positive behaviour support plan examples.

Table of Contents
What does discrimination mean in health and social care?
Positive behaviour support is a proactive, person-centred approach to helping a client. It involves working to understand the reasons behind their behaviour, and adapting their environment to improve their quality of life.
Positive behaviour support assumes that a client’s challenging behaviour is happening for a reason.
Some people might display challenging behaviour if they can’t communicate their feelings, needs and wishes – especially if they have learnt that it brings results in the past.
For example, an individual might hit other people when they want to leave a group activity. Alternatively, some clients might crave the sensory experience of some behaviour, such as eating inedible objects or breaking things.
Using PBS, carers attempt to change the client’s environment to support the person better, and teach new, less harmful, behaviours where possible.
Some positive behaviour support examples might include:
- John often bangs his head against his bedroom wall. This is because he doesn’t like the bright overhead lights in his bedroom. He only bangs his head when they’re turned on. His carer could replace the bulbs with less bright ones, or install a dimmer switch and teach John how to use it.
- Katie attends an art class with other young people at her care facility. When she is there, she sometimes hits teachers, carers, and other residents. She has learnt that when she hits, her carer takes her out of the activity room, so she now starts to hit when she wants to go back to her room. Her carer could teach her an alternative method to ask to leave the group – perhaps using sign language, or holding up a card. Her care team could also learn to look for early warning signs that Katie is ready to go home – she might stand up or put her paintbrush down.
- Will often tries to eat objects that are not edible, like stones or coins. He enjoys the sensation of chewing these objects, and does not understand the health risks involved. His carers could look for safe foods that give similar sensory feedback, and make those easily accessible to him.
PBS means finding constructive and person-centred solutions to challenging behaviours, while supporting a client’s independence and dignity. It should not involve punishment.

What is challenging behaviour?
Challenging behaviour might include:
- hurting other people, such as hitting or biting
- self-injury, such as head banging or biting hands
- eating things that are not edible, like bedding or books
- destructive behaviours, such as throwing items or breaking furniture
- other inappropriate behaviour, such as spitting or removing clothes
Anyone can display challenging behaviour, but it is often seen in individuals with learning disabilities or communication difficulties.
Support better behaviour. Support better lives. 💜
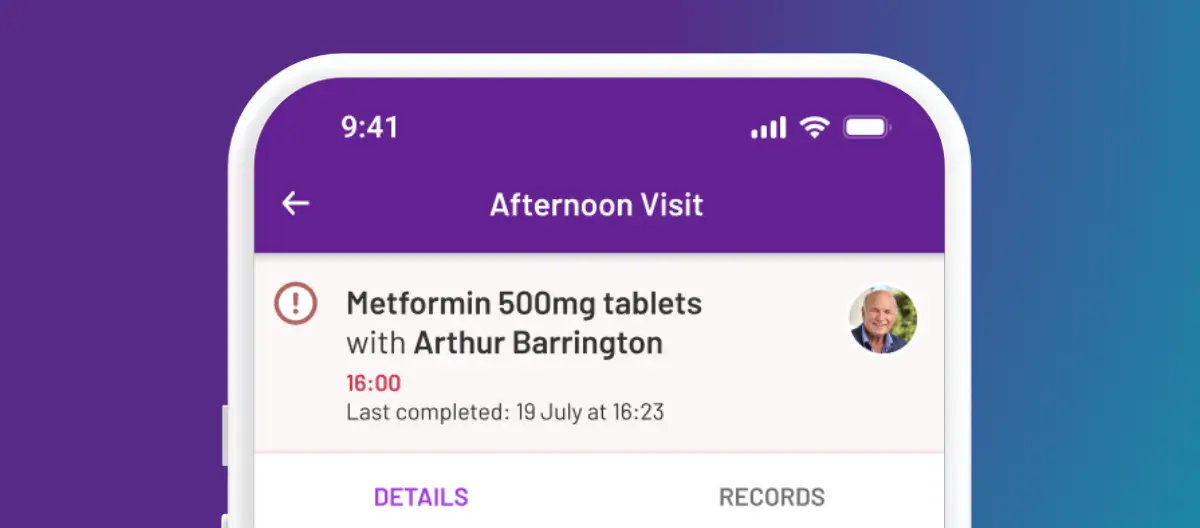
Positive behaviour support works best when everyone is on the same page. PASS makes it easier to record behaviours clearly, spot patterns early, and share updates with the whole care team in real time.
With accurate notes, smart observations, and secure family communication, PASS helps you understand what a person is trying to communicate and respond in the right way at the right time.
Book a tour today to see how PASS can support safer decision making and calmer days for your clients and your team.
What is a positive behaviour support plan?
A positive behaviour support plan is a document that can help carers implement PBS. It should provide carers and family members with the information they need to understand a client’s behaviour, and know what to do to support them.
The plan should include information about the challenging behaviour, the reasons behind it, and any early warning signs. It should explain how carers can help to diffuse a difficult situation before the client becomes too distressed, if possible. If the client does display challenging behaviour, the PBS plan should advise carers how to act.
PBS plans may refer to different stages or zones of behaviour:
- Green: calm, relaxed and happy
- Amber: showing early warning signs of distress
- Red: distressed and in crisis, displaying challenging behaviour
- Blue: calming down after the crisis, but may still feel distressed
A positive behaviour support plan should include both proactive and reactive strategies.
- Proactive strategies can help to improve a client’s quality of life on a day-to-day basis – keeping them in the green zone more of the time. The plan should include information about the client’s likes and dislikes, and how their carers can tell if they’re feeling happy and relaxed. Proactive strategies might include making changes to a client’s environment, or teaching them signs so they can request to leave a group setting, ask for food, or talk about pain.
- Reactive strategies can help carers keep the client safe when they are showing early warning signs or displaying challenging behaviour – or in the amber or red zones. The plan should describe early warning signs so that carers can attempt to de-escalate the situation, and explain the best ways to do this. Reactive strategies might include attempting to distract or redirect the client, or taking away a trigger. Restrictive strategies, such as physical restraints or medication, should only be used as a last resort.
A PBS plan should include more proactive strategies than reactive.
Who should use a positive behaviour support plan?
Positive behaviour support can help any clients with challenging behaviours. It is most commonly used to support people with learning disabilities, and may also be used to help autistic clients. Positive behaviour support plans are tailored to each client, so they even can be used for children, or clients with severe learning disabilities.
If a client has a PBS plan, it should be used everywhere they go. This might include their home or care home, day centre or respite care facility, school, and out in the community.
Everyone who supports the individual should use the approaches outlined in the plan, whether they are care workers, family members, or teachers. This gives your client consistency, and also allows you to see what strategies work best. Family and friends may need some PBS training if they are unfamiliar with the concept.
If your client is supported by paid carers and family members, you can discuss their care easily with home care software that supports secure messaging.
The secure messaging service allows you to communicate directly with a service user’s family or friends in real time, so you can share information about behaviour, medication, and other crucial care activities.

Who can write a positive behaviour support plan?
A clinical psychologist or behavioural specialist might write your client’s positive behaviour support plan. They will carry out a functional assessment, where they look at the reasons behind their behaviour.
However, if a service user is waiting for an assessment, a care provider might urgently need to understand their needs and manage challenging behaviours. In these situations, as a care provider, you may need to produce a positive behaviour support plan for a client.
Steps to writing a positive behaviour support plan:
- Start by observing your client’s behaviour. How do they act when they are happy? What are their early warning signs? What challenging behaviour do they display? Use an ABC chart to record their behaviour, and look for trends and reasons.
- Look for changes that can improve your client’s quality of life. Consider whether you can provide an alternative behaviour for your client, or make changes to their environment to reduce their distress. These changes can help to keep them in the green zone for longer.
- Look at how you can de-escalate early warning signs and challenging behaviour. When they’re in the amber or red zones, how can you diffuse the situation?
- Consider what help your client needs after a crisis, when they’re in the blue zone. Some people will calm down quickly, but others may need extra support.
Producing a positive behaviour support plan should be a group effort. You should look for input from anyone who supports your client or spends a lot of time with them.
As with all care planning software, the best results come from insights gathered from everyone involved in care and daily life.
This might include:
- Family members and close friends, if appropriate
- Carers, activity support workers, and other members of staff at any residential or day facilities your client attends
- Teachers and learning support assistants, if your client attends school
PBS training could be valuable to you and your staff team, especially if you support multiple clients who display challenging behaviours.
If you need to write a positive behaviour support plan, PBS training might be especially useful. You may be able to find more information from Skills for Care or the Challenging Behaviour Foundation.
Positive behaviour support plan template
A positive behaviour support plan template should include a description of the difficult situation for the client, and the behaviour that they might display. It should talk about the signs that the client is happy, some early warning signs, the crisis behaviour, and how they may react afterwards – and how carers should react to each stage of behaviour.
Let’s look at a template positive behaviour support plan. We’ll use one of the examples of challenging behaviour that we discussed earlier.
Client name: Katie
Difficult situation: Art class, particularly near the end of the session
Green zone behaviour: Katie smiles and sings a lot when she is happy and calm. She might be engrossed in her painting, or take small breaks where she wants carers and other residents to look at her artwork.
How to keep Katie in the green zone: Before the art class, make sure that Katie knows she can ask to leave at any time. Remind her of the sign for “home”, and check that she has her cards. During the class, keep talking to Katie about her painting and encouraging her.
Amber zone behaviour: Katie might put her paintbrush down or stand up and sit down several times. She might stop smiling and seem very tense.
How to respond when Katie is in the amber zone: Ask Katie if she wants to leave the session. Reassure Katie that she can finish her painting during the next class. Distract Katie by starting to sing one of her favourite songs – she may join in.
Red zone behaviour: Katie might shout or cry, or hit her carer or other residents.
How to support Katie when she is in the red zone: Talk calmly to her. If she moves her hands to hit someone, say, “Kind hands.” Encourage her to move away from the table and other residents and carers. Start singing one of her favourite songs – she particularly likes songs by Abba.
Blue zone behaviour: Katie might be very upset. She might be weepy or want a hug from a trusted carer.
How to support Katie afterwards: Give Katie a hug if she requests one. Sing with her and encourage her to have a snack and a drink.
Remember, a positive behaviour support plan should be a true example of person-centred care, and there is no one-size-fits-all solution. You can look at positive behaviour support plan examples, but the plan for your client should be tailored directly to their needs and preferences.
How do we know if a positive behaviour support plan is working?
You can tell that a positive behaviour support plan is working for your client if you notice a reduction in the frequency or severity of their challenging behaviours.
They may still display challenging behaviours – but if they happen less often, are less severe, or last for a shorter duration, the PBS plan may be working for them. The client might also seem more relaxed, happier, or more willing to take part in activities.
Positive behaviour support is not a quick fix. You might not notice changes at first. It’s important to collect data on your client’s behaviours, so that you can document progress and know what works for them.
As with all care plans, you should review a positive behaviour support plan regularly, and update it if necessary. Your organisation might have a suggested review cycle, or you might choose to include it with your regular care planning reviews.
However, if your client is increasingly distressed or is displaying more challenging behaviours, you may need to review and amend the PBS plan more urgently. If you often need to use reactive strategies, such as medication or physical restraint, you should also look at whether the plan needs to be updated.
Conclusion: positive behaviour support plans
Positive behaviour support plans can be a useful tool to help clients who display challenging behaviour.
As a care provider, you know that this behaviour often comes from distress or difficulty communicating. Positive behaviour support involves getting to the reasons behind the behaviour, and making changes to help your client to remain happy and calm where possible.
Positive behaviour support should be proactive, and should never be about punishing a client for their behaviour. Instead, it should focus on improving a client’s quality of life, and improving their skills if possible.