When a client is nearing the end of their life, they’ll need a high level of support.
An end of life care plan will explain their needs and wishes, ensuring that their care team know how to look after them.
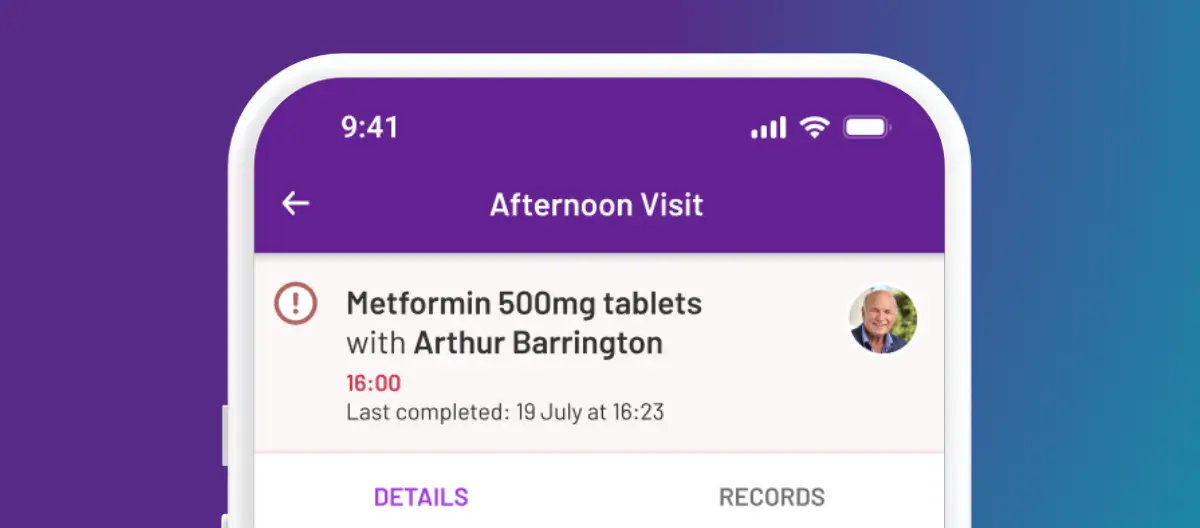
If you’ve never supported someone at the end of their life before, preparing an end of life care plan might feel daunting. However, care planning software can simplify the process.
In this guide, we’ll look at what end of life care is, what is included in an end of life care plan, and how to write an end of life care plan. We’ll also talk about how you can plan for end of life care for yourself or a relative.

Table of Contents
What is end of life care?
Before we talk about how to write an end of life care plan, we should define end of life care. This is the support that a client receives towards the end of their life – this could be days, weeks, or months.
End of life care focuses on helping a client to live well. Even though they won’t recover from their illness, end of life care tries to ensure that they are comfortable. It can be delivered in the individual’s own home, a care home, hospital or hospice.
End of life care will look different for each client, depending on their health condition, family situation, and individual wishes. However, it often involves:
- Personal care, such as washing, dressing, and support with feeding
- Managing pain, nausea, breathlessness, and other symptoms
- Providing emotional support
- Supporting family members and other loved ones
- Helping the client and their family with administration
As a care worker providing end of life care, you’ll be part of a larger team. Other people involved might include your client’s GP or specialist doctor, community nurses, pharmacists, occupational therapists, hospice staff, and chaplains or religious leaders.

What is an end of life care plan?
An end of life care plan is a document that explains a client’s needs, wishes, and medical requirements at the end of their life.
It explains how an individual’s carers, family, friends, and healthcare team can support them in their last days and weeks.
Remember, there’s no one-size-fits-all solution for end of life care – it should be a continuation of person-centred care. You may have an end of life care plan template, but the details included should be tailored to each service user, and reflect their circumstances and preferences. For example, an end of life care plan for a nursing home resident with dementia might look different to one for a client with motor neurone disease who lives in their own home.
End of life care plans can help to ensure that your client’s wishes and dignity are respected at the end of their life. For example, if they would prefer to die at home, rather than in hospital, the care plan can record that. Their care team can then
You might use care management software to record the details, print out a hard copy, or have an end of life care plan PDF document that necessary staff and close family can access.
It’s important that a client’s end of life care plan is easily accessible, but also kept securely – other clients, unauthorised family members, and visitors should not have access to it. A friends and family portal such as openPASS can keep a client’s support system connected, helping them feel included and allowing you to provide the best end of life care possible.

What is included in an end of life care plan?
A good end of life care plan should include:
- Important personal details, such as the client’s legal and preferred names, date of birth, and preferred language or method of communication. If someone has lasting power of attorney for your client, these details should also be included.
- Medical details, including any current health conditions and medication they need.
- Needs and preferences around symptom management, such as how to handle pain, nausea, and breathlessness.
- Advance directives and wishes about medical treatment, including any advance decisions to refuse treatment (ADRT). While many of the details in an end of life care plan are merely preferences, an ADRT can be legally binding. If your client has an ADRT, it’s important to make sure that their care team and other healthcare professionals are aware of it.
- Preferences about emotional support, such as counselling and support from religious groups.
- Religious, spiritual, or other requirements, which may include needs involving prayer, diet and washing, as well as what to do after the client has died.
- Preferences about location, such as whether your client prefers to remain at home, in their care home, or move to hospice or a hospital.
- Details about the client’s wider support system, such as family members and close friends. They may also need support during their loved one’s illness and after the death.
- Emergency contact details, which may include family members, healthcare professionals, and spiritual advisors.
- Details about when the plan should be reviewed.
Support your team to deliver compassionate end of life care with PASS 💜
Caring for someone at the end of their life takes time, empathy, and clear communication. PASS helps carers focus on what matters most: comfort, dignity, and peace of mind for every person in their care.
With personalised care plans, real-time updates, and shared notes, your team can work together seamlessly to provide consistent, person-centred support, even in the most sensitive moments.
Book a tour today to see how PASS can help your carers deliver truly person-led end of life care.
Who writes an end of life care plan?
If you work in a care home or provide domiciliary care for a client, you may be involved in preparing an end of life care plan.
The care plan should involve discussion between:
- The client
- Their close friends and family, if appropriate
- Their carers
- Their GP or specialist doctor
- Community or palliative care nurses
- Hospice staff, if appropriate
- Religious leaders, spiritual advisors, or counsellors
However, if you are the client’s main care provider, you may need to take the lead in preparing the end of life care plan. If you’ve never written one before, your client’s healthcare team may be able to provide you with some end of life care plan examples. For clients who are accessing hospice care, the specialist staff there may have resources to support you.

When does a client need an end of life care plan?
You should prepare an end of life care plan when a client is nearing the end of their life, but while they are still able to discuss their wishes with you.
You might write an end of life care plan for a client in these situations:
- When their healthcare team believes they are expected to die within 12 months
- When they have an incurable illness, such as motor neurone disease or advanced cancer
- After a catastrophic medical event, such as a stroke or serious accident
- If they have a medical condition that means they may die suddenly
Your organisation’s policies and procedures may have other guidelines that explain when you should produce an end of life care plan. For example, some organisations might ask all new clients about their wishes around end of life care, even if they are currently in good health.
Like all care plans, end of life care plans should be regularly reviewed, especially if there is a change in the client’s circumstances or health condition. If your client is not able to share their wishes, close family members and friends may be involved in these reviews and discussions, if appropriate.
How to talk to clients about end of life care
It can be difficult to talk about dying. Even if a client has an incurable diagnosis, they may be resistant to discussing end of life care – and the same might be true for their family and friends.
It’s understandable that people want to avoid the conversation – after all, it can bring up many uncomfortable feelings. However, it’s important to start the conversation, so that you can learn about a client’s wishes, help reduce their anxiety, and support them to make practical decisions.
How to talk to clients about end of life care plans:
- Be ready to talk about the topic when your client is. If they bring the topic up, be willing to engage with them.
- Check what they already know about their condition.
- Ask direct questions about their wishes – for example, “When you are very ill, who do you want to be with you?”
- Answer questions honestly. Your client may ask whether they will get better, or what will happen to their body after they die. If you don’t know the answer, be honest, and talk to other healthcare providers if necessary.
- Avoid using euphemisms such as pass away – instead, use direct words such as die. This is especially important for people with learning difficulties or who may struggle to understand.
- Give them your full attention when having these conversations. If you’re scheduling time for an end of life care planning meeting, make sure you allocate time for a full discussion.
If you’re a care manager, you could invest in end of life care training for your team. For example, the Gold Standards Framework provides training for staff who deliver care to people nearing the end of their life.
How can I plan for end of life care?
If you’re facing a terminal diagnosis yourself, or support a friend or family member who is dying, you might need to plan end of life care.
When you’re preparing an end of life care plan for yourself or a loved one, you should ask yourself some questions about preferences, and make sure that the answers are clearly written down. Consider whether you would like to stay at home or go into hospital, how you want to manage your symptoms, and who you would like with you.
Questions to ask when preparing an end of life care plan:
- What symptoms am I likely to experience, and what treatment would I like for them?
- Are there any treatments I would like to refuse?
- As my condition deteriorates, will I need personal care or additional support, and who will provide that for me?
- Who will I lean on for emotional support?
- Who supports me to make decisions?
- Who do I want to be with me when I am very ill or dying?
- Where do I want to be when I am very ill or dying?
- What do I want to happen if I can no longer make decisions about my care?
You may need to discuss these questions with your healthcare team, close family members and friends. If you have support from carers in your home, or live in a care home, your care worker or a supervisor may be able to help you answer these questions.
Conclusion: What is an end of life care plan?
An end of life care plan details a client’s needs and wishes for the end of their life. It should be produced through discussion with the client, their close friends and family, healthcare professionals, and their care team.
A good end of life care plan should include information about the individual’s condition, how they would like to manage their symptoms, who they want with them for emotional support, and where they would like to die.
Preparing an end of life care plan can help you ensure that you understand your client’s priorities, and allow you to support them to have a good death.