For care providers in England, CQC inspections play a crucial role in assessing care quality and regulatory compliance.
A strong rating not only affirms the quality of service being delivered but also impacts reputation, funding opportunities, and staff retention.
Despite this, many providers focus on last-minute preparation when the key to success is integrating compliance into everyday care delivery. By following a proactive approach, care organisations can confidently navigate inspections and showcase the outstanding, person-centred care they provide.
In this article, we’ll take a look at how the right planning can help care providers pass CQC inspections with confidence, including expert-backed insights and a practical checklist to keep your organisation inspection-ready at all times.
Article by:

Taffy Gatawa, Chief Information & Compliance Officer at PASS
Taffy is a key member of our Senior Leadership Team, providing strategic guidance on compliance and regulatory standards. With a clinical background in nursing and hands-on experience in both Mental Health and General Medicine, Taffy has worked across the NHS and private sector, equipping care providers with the knowledge and tools to navigate the complexities of CQC regulations.
Table of Contents
Preparing for an inspection: What CQC looks for
The key to a stress-free CQC inspection isn’t reactive preparation but embedding compliance into everyday operations to show that person-centred care is at the heart of service delivery.
CQC inspectors assess care services across five key areas:
- Safe: Are people protected from harm and abuse?
- Effective: Does care, treatment, and support achieve good outcomes?
- Caring: Do staff involve and treat people with compassion and respect?
- Responsive: Are services organised to meet people’s needs?
- Well-led: Is leadership strong and fostering a culture of quality and safety?
Inspectors want to see these policies actively implemented and will speak with staff, people in care, and family members to ensure that day-to-day operations align with documented procedures. This means that leadership, frontline staff, and even service users need to be prepared to confidently discuss the service’s approach to care quality.
Expert insight 💡
Many care providers think inspections are about showcasing paperwork, but what truly matters is how well staff understand and apply compliance processes. A well-prepared team that can confidently explain procedures to inspectors makes a significant difference.
Common compliance mistakes that lead to lower ratings
Even the most well-managed care services can make common compliance mistakes that negatively impact their CQC ratings. Identifying and addressing any issues that may arise early can prevent avoidable setbacks, help to maintain a high standard of care, and ensure providers are always inspection-ready.
- Documentation gaps: If records are incomplete, outdated, or inconsistent, providers struggle to evidence quality care. This can lead to questions about care continuity and regulatory compliance.
- Staff knowledge gaps: Employees may be unfamiliar with policies, leading to inconsistent practices. If staff members cannot confidently explain safety measures, medication protocols, or safeguarding procedures, it raises red flags.
- Lack of real-time compliance tracking: Without automated compliance monitoring, errors often go unnoticed until it’s too late. Reactive approaches to compliance can make services appear disorganised and unprepared.
- Data security concerns: Paper-based or outdated digital systems create risks for confidentiality breaches and regulatory non-compliance. Inspectors expect care providers to have robust data security measures in place.
Expert insight 💡
Even small compliance gaps can raise red flags during an inspection. In addition to reviewing documentation, inspectors will ask staff about processes, look at training records, and assess how well the team can demonstrate that best practices are followed for daily care.

The value of embedding person-centred practices into daily compliance
CQC inspectors are increasingly focusing on how a provider has built their care processes around each person’s unique needs and preferences rather than relying on one-size-fits-all processes.
To truly make person-centred care into daily practice, providers should:
- Involve clients in decision-making to ensure that their preferences are factored in shaping care plans.
- Leverage the full capabilities of digital tools to assist with documenting personal goals, routines, and evolving needs in real time.
- Train staff to recognise and support individual choices, communication preferences, and autonomy.
- Regularly review digital care plans with input from the person receiving care and their loved ones.
Expert insight 💡
Inspectors want to see evidence of care that adapts to the individual needs of clients. Providers who actively engage clients to better understand and improve their care consistently achieve higher ratings.
How to stay inspection-ready at all times
Outstanding providers don’t prepare for inspections at the last minute. Instead, they build compliance into their daily workflow using a proactive approach that ensures an inspection is just another routine review rather than a major event requiring excessive preparation.
To stay inspection-ready, providers should:
- Verify that care plans and risk assessments are continuously updated and reflect current best practices.
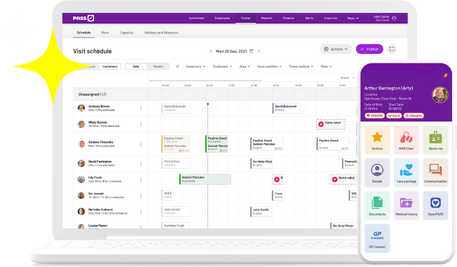
- Use real-time compliance tracking tools, like PASS care management software, to spot and fix gaps proactively before they become issues.
- Conduct regular internal audits to ensure that all documentation is up to date and aligned with regulatory standards.
- Foster a culture of continuous learning, ensuring that staff regularly engage in training and reflective practice.
Expert insight 💡
One of the biggest indicators of a well-led service is a culture of continuous improvement. If compliance is only reviewed before an inspection, it’s likely not ingrained in daily operations.
The role of staff training and confidence in CQC inspection success
A care provider’s CQC rating is heavily influenced by its workforce. Well-trained, confident staff members who can articulate their roles and responsibilities during an inspection leave a strong impression on inspectors.
To ensure staff are well-prepared:
- Provide ongoing training to ensure employees understand policies and procedures and can confidently apply them.
- Conduct mock inspections where staff practice answering common CQC questions.
- Encourage staff to reflect on their professional development and how they contribute to quality improvement.
Expert insight 💡
Inspectors will ask staff how they contribute to quality improvement. Providers that support their teams often receive higher ratings because compliance is seen as a shared responsibility, not just a management concern.
What sets outstanding providers apart
Care providers that consistently achieve ‘Outstanding’ ratings share key characteristics:
Strong leadership: Leaders set the tone for a culture of quality and accountability.
Continuous improvement: Services proactively seek feedback and act on it.
Technology adoption: Digital solutions streamline compliance and operational efficiency.
Staff empowerment: Employees feel valued, well-trained, and motivated to provide the highest level of care.
Expert insight 💡
Inspectors are looking for a provider that doesn’t just meet minimum standards but actively seeks to exceed them. The difference between ‘Good’ and ‘Outstanding’ is a provider’s commitment to going beyond compliance and truly embedding excellence.
Looking for leadership content? Check out our Leadership Hub today and access free resources and training materials.
The role of technology in CQC inspection readiness
Having a digital system that continuously collects and organises compliance data not only ensures a smoother inspection process but also allows providers to focus more on delivering quality care rather than chasing paperwork.
Digital compliance tools, such as PASS, provide care providers with:
Automatic documentation tracking: Care records are updated in real time, reducing the risk of missing crucial evidence.
Audit-ready reports: With one click, managers can generate detailed compliance reports aligned with CQC expectations.
GP Connect integration: Ensuring instant access to patient data, improving care coordination and evidencing proactive management.
Incident tracking tools: Providing a clear record of how the service identifies, addresses, and learns from issues.
Expert insight 💡
Providers who embrace digital compliance tools often achieve better ratings because they can instantly provide clear, verifiable evidence to inspectors. These tools also demonstrate a commitment to person-centred care by showing the level of individualised support provided to each client at any given time.
Want to see if a digital care management tool like PASS is right for your service? Take the 60-second quiz now.

A checklist for a stress-free CQC inspection process
A smooth CQC inspection starts with having the right processes in place before an inspector arrives. By regularly reviewing and updating key areas of compliance, care providers can ensure they’re always prepared.
Use this checklist to assess whether your team is inspection-ready:
- Care plans are up-to-date and personalised.
- Risk assessments are regularly reviewed and documented.
- Compliance data is stored securely and easily accessible.
- Staff training records are maintained and up to date.
- Incident reports include clear records of corrective actions.
- Audits are carried out routinely, with evidence of improvements.
- Clients and families are engaged in care planning decisions.
- Staff are confident in explaining procedures and best practices to inspectors.
Expert insight 💡
Providers who prepare for an inspection as if it were happening tomorrow, every day, eliminate the stress of last-minute preparation.
Did you know you can make digital checklists like this in PASS? Learn more here.

Closing thoughts
When compliance is embedded into everyday practice, CQC inspections become an opportunity to demonstrate the quality of care your organisation provides for its clients rather than a source of stress.
Technology plays an increasingly important role in ensuring documentation reflects real, meaningful care and in developing a well-trained, confident workforce that is always inspection-ready.
By fostering a culture of continuous improvement, care organisations can stay ahead of regulatory requirements and focus on delivering the best possible outcomes for the people they support.