As we age, our sleep patterns often change. Excessive sleeping in elderly clients isn’t uncommon – and others might find it difficult to sleep at all.
As a carer, you’ll come to learn your clients’ usual sleep patterns. Maybe they sleep for nine hours each night and never in the day, or perhaps they prefer to have several long naps and a shorter sleep at night.
Depending on their needs, you might need to support service users in getting ready for bed and creating a good environment for sleep.
Having the right care management software in place can help you keep track of sleep-related support needs, spot patterns, and tailor care accordingly.
In this article, we’ll look at why sleep is important for older people, sleep patterns by age, when to be concerned about too much or too little sleep, and how you can help your clients rest well.

Table of Contents
Why is sleep important for the elderly?
Sleep is important for all of us. Adults should generally try to get between seven and nine hours of sleep each night – although some people may have different sleep needs.
We need sleep so that our body can stay healthy and we can be alert during the day.
When people struggle to sleep, it’s called insomnia.
Some of the symptoms of insomnia might include:
- Struggling to get to sleep
- Waking often during the night
- Waking up very early and not being able to go back to sleep
- Being unable to nap during the day, even if you’re tired
So, how does a lack of sleep affect the elderly in particular? If your client is struggling with insomnia, what are the effects?
You’ll have noticed how tired you feel after a poor night’s sleep. You might be irritable, struggle to concentrate, or just feel like you’re going to drop off all day. Sleep for the elderly is no different. If your older clients aren’t getting enough sleep at night, they’ll be extra tired during the day.
They may also struggle with their co-ordination – which could increase their risk of falls and injuries.
Not only that, but being sleep deprived can increase the risk of conditions like high blood pressure and diabetes. As older people are more at risk of these conditions anyway, it’s important to make sure that they’re getting enough sleep.

Age and sleep patterns
There are often changes in sleep patterns by age. For example, we usually need more sleep when we’re young.
- Babies under one year old: 12-16 hours per day
- Children between one and two years old: 11-14 hours per day
- Children between three and five years old: 10-13 hours per day
- Children between six and 12 years old: 9-12 hours per day
- Teenagers between 13 and 18 years old: 8-10 hours per day
- Adults over 18 years old: 7-9 hours per day
Unfortunately, aging and sleep can be a tricky combination. Even though older adults may need the same amount of sleep as when they were younger, they might find that their sleep patterns have changed.
For example, many older people go to bed earlier and get up earlier than they did in the past. They often wake up more often during the night, and some people find that they’re more easily disturbed than they used to be.
Sometimes, there are clear reasons behind this – for example, exercising less, being in pain, or being very anxious. But other times, it’s not so easy to work out the reasons. As a carer, though, you should talk to your clients about their sleep, and ask if there are ways you can help them.
How can I help my clients sleep well?
As a carer, you’ll probably need to support some service users with getting ready for bed. During these care visits, you should check in with them about their sleep habits. Do they have trouble sleeping? What is their nighttime routine like?
You might not be able to fix all of your clients’ sleep issues, but there are some things you can do to support them.
Tips for helping clients get a good night’s sleep:
- Encourage them to follow a bedtime routine. During the care planning process, try to make sure that their care visits are at a consistent time, especially if they need support with getting ready for bed. Using care planning software can make it easier to build and update personalised routines that promote better sleep and wellbeing.
- Encourage them to go to the toilet before bed. Lots of older people wake up in the night because they need to urinate. This is especially common in older men.
- Encourage them to relax before bedtime. This could involve reading a book, taking a bath, or listening to quiet music. For some people, watching TV or using a computer or phone before bed can make it harder to sleep.
- Support them to exercise or get outside regularly. Spending time in nature can help people sleep well, and exercise will help them feel tired.
- Encourage them to avoid napping. If your client naps during the day but struggles to sleep at night, suggest that they change their routine. Naps in the late afternoon and evening will make it especially hard to sleep at night.
- Make sure that their bedroom is a good temperature and their bed is comfortable. Being uncomfortable will make it harder for your clients to sleep.
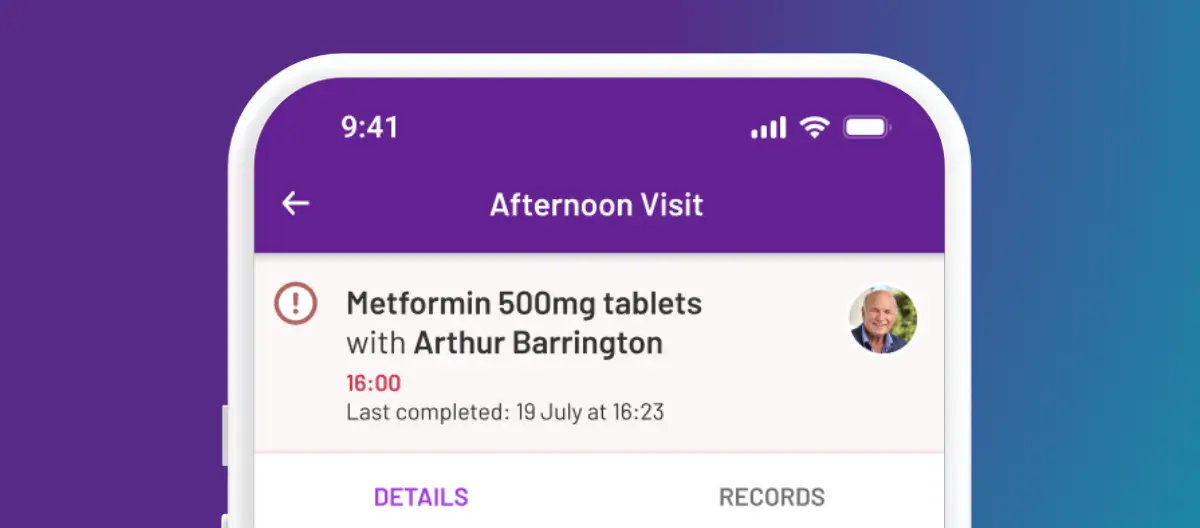
- Make sure they’ve taken any necessary medication. If they’re in pain or discomfort, they may not be able to sleep easily. If their medication makes it harder for them to sleep, encourage them to talk to their healthcare team about the side effects – they shouldn’t stop taking prescribed medication without discussion. Make sure that you note down any medication changes in your eMAR
- Encourage them to avoid too much caffeine, especially in the evening. Some clients may like to switch to drinking caffeine-free tea or coffee, or they may prefer to try different drinks. Remember that caffeine is also found in lots of chocolate-based food and drinks, so hot chocolate before bed might make it difficult for your clients to sleep.
- Avoid preparing large meals for them in the evening. Good nutrition is important for your clients, but encourage them to eat their bigger meals earlier in the day.
If they’re still struggling with sleep, advise them to talk to their GP or pharmacist about their sleep problems.

When should I be concerned about a client’s sleep?
It’s normal for sleep habits to fluctuate, especially if a service user is ill or has had a change in routine.
A few sleepless nights or very tired days are usually nothing to worry about – as we’ve mentioned, seniors and sleep can sometimes be a challenging combination. But sometimes, worrying sleep patterns can last for a long time.
Does your client wake refreshed and ready to face the day? If they do, then they’re probably getting enough sleep.
But if they’re tired and feel lethargic during the day, they might not be getting enough good quality sleep – even if they’re sleeping for the recommended 7-9 hours per day. Alternatively, there could be an underlying health issue that’s causing their tiredness.
Ask yourself the following questions:
- Have the sleep issues been going on for longer than a few days or weeks?
- Is my client tired and confused during the day?
- Did the sleep issues start when my client started a new medication or activity?
- Does my client seem depressed or anxious?
- Is my client in pain or discomfort?
- Does my client need to use the toilet during the night more than usual?
If you’ve answered yes to any of these questions, there might be cause for concern.
If you’re worried about excessive sleeping in elderly clients, or think that a client isn’t getting enough sleep, talk to them about your concerns. You may need to support them to speak to their GP or healthcare team.
What is not enough sleep?
Lots of older people struggle to get enough sleep.
There are a few reasons that your clients might not be able to sleep, including:
- Being less active
- Discomfort, pain or nausea that disturbs them
- Medications causing insomnia
- Anxiety and depression
- Being aware of noises around them, especially if they’ve recently moved

But you should try to help your clients get at least six hours of sleep each night. Staying busy during the day can help. Even if your service users aren’t able to be very energetic, activities like art therapy can encourage relaxation and potentially improve sleep.
- Make sure they always have a drink within reach.
- Offer a variety of drinks, such as water, squash, tea and coffee.
- Try different cups, glasses or bottles. Some clients may prefer to drink from a straw.
- Sit with them and have a cup of tea yourself.
- Provide foods with high water content, such as watermelon and soup.
Causes of excessive sleepiness in elderly people
Why do elderly people sleep so much? It’s normal to sleep more sometimes. For example, if your client is ill or has been extra active, they might be extra tired.
But excessive sleeping in elderly people can be a sign of other problems, including:
- Depression
- Chronic fatigue syndrome
- Anaemia
- Other health conditions, such as Parkinson’s or epilepsy
- Drinking too much alcohol
- Side effects from medication
It could also be a sign that your client isn’t getting good quality sleep – for example, if they have sleep apnoea, restless leg syndrome, or need to get up to use the toilet a lot during the night.
Whatever the reason, if a service user is noticeably more tired than usual for a period of time, encourage them to talk to their GP for advice.
If your client is receiving end of life care, their illness and medications might make them excessively sleepy. Depending on their condition and symptoms, their healthcare team may be able to make changes to their medication plan so that they can feel more awake and have a better quality of life.
Conclusion: Seniors and sleep
A lack of sleep or excessive sleeping in elderly clients can be worrying for care workers.
As a carer, you should be able to support your clients with a comforting and relaxing bedtime routine, and be there for them if they need to talk about their worries.
It’s normal for people’s sleep patterns to change as they age, but sometimes you may need to encourage your service users to seek help.
Good home care software helps carers spot these changes early and respond in a timely, well-documented way.
If the change in their sleep patterns was sudden, if they’re distressed by a lack of sleep, or if they’re no longer able to be alert and awake during the day, there may be a cause for concern.