Whether you work in domiciliary care or support people in a care home, your clients may be at risk of pressure ulcers.
The Waterlow Score can help you assess their chance of developing pressure sores, so you can take action to keep them safe.
Pressure ulcers can be painful, and lead to complications such as reduced mobility, infection, and hospitalisation. As a good care provider, it’s important to identify whether your clients are at risk, and help them avoid developing pressure sores and their associated complications.
In this article, we’ll look at what the Waterlow score is and what it’s used for, how to calculate Waterlow Score results, and the steps you should take to keep clients safe from pressure sores.
Want to calculate now? Use our free online Waterlow Score Calculator.

Table of Contents
What is a Waterlow Score?
The Waterlow Score helps care providers assess a client’s risk of developing pressure ulcers.
This means that you can take action to help the client avoid pressure sores and their possible complications. The risk assessment tool was developed in 1985 by Judy Waterlow, a clinical nurse tutor.
When looking at someone’s Waterlow Score, you need to consider seven major risk factors. These factors look at how likely the client is to develop pressure sores – and whether there are issues that could impact recovery.
A client is given a score in each category.
What are the Waterlow Score factors?
- Sex and age: Women have a higher risk of developing pressure ulcers, as do older adults.
- BMI, or build and height: This allows you to work out whether your client is overweight or underweight. People who are overweight or malnourished are more likely to develop pressure ulcers or take longer to recover. If you need to work out a client’s BMI, you can use the tool on the NHS website.
- Skin condition: If a client’s skin is already showing signs of pressure damage, they are more at risk. Alternatively, if they have other wounds, injuries, or fragile skin, they may have a higher chance of developing pressure ulcers.
- Continence: Clients who have continence issues are more at risk of pressure sores. Whether they struggle with urinary or faecal continence, their skin will be exposed to moisture more often.
- Mobility: Clients with reduced mobility are often at the highest risk of developing pressure ulcers, especially if they can’t easily turn or reposition themselves in their bed or chair.
- Appetite and nutrition: If a client is dehydrated, malnourished or on a very restricted diet, they may have a higher chance of pressure sores. Additionally, they may also take longer to recover from injuries.
- Additional factors: Depending on your client’s health conditions, there may be other factors that can raise their risk of developing pressure ulcers. For example, a prosthetic limb adds another potential area of pressure, or diabetes could affect overall skin health. Some cancer drugs and blood thinners can also increase the risk of pressure sores, as can smoking.
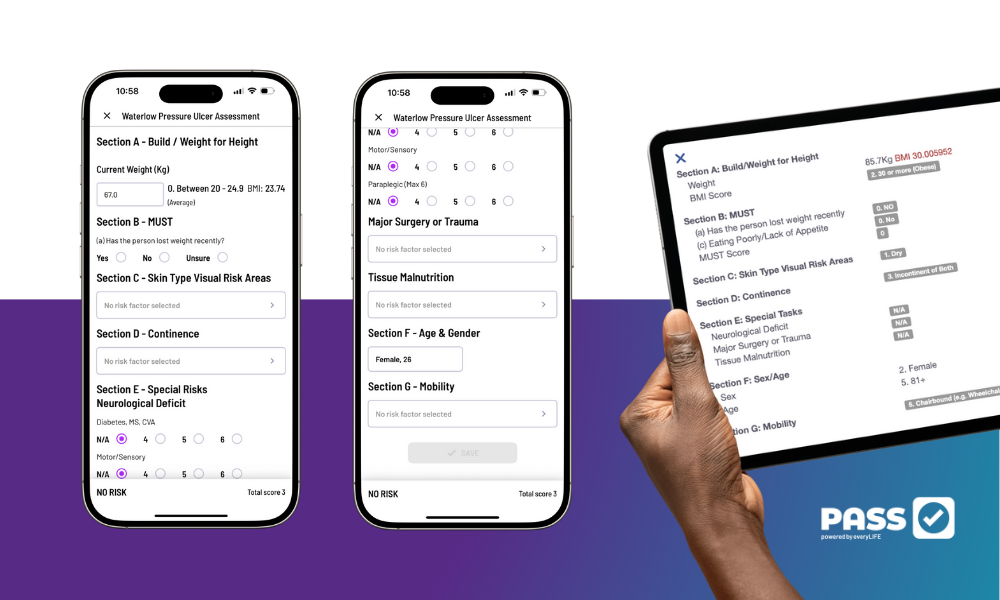
Simplify your Waterlow Score assessments with PASS 💡
PASS includes easy-to-use digital tools, like the Waterlow Score, to streamline assessments, track risks, and protect your clients from pressure ulcers.
Book a tour today to see how PASS can simplify care planning for your organisation.
Who should use the Waterlow Score?
Whether you work in domiciliary care or support people in a care home, you should use the Waterlow Score to work out the risk of clients developing pressure ulcers.
You should do this as part of your care planning and risk assessment processes for each service user, whatever their age. Even babies, children and young people can develop pressure ulcers, depending on their health and mobility.
NICE guidelines say that pressure ulcer risk assessments should be carried out for clients of all ages, if they have any of these risk factors:
- limited mobility
- an inability to change positions
- loss of sensation (feeling)
- a restricted diet or nutritional deficiencies
- a previous pressure ulcer
- cognitive impairment
Depending on your organisation’s policies and procedures, you might carry out a risk assessment on all new clients who will receive personal care. If you work in a nursing home, you should carry out a risk assessment within six hours of the client moving in.
The Waterlow Score is also used by the NHS to assess whether patients are at risk of developing pressure ulcers.
Pressure ulcer risk assessments should be repeated regularly, especially if your client’s health condition changes.

What are pressure ulcers?
Pressure ulcers might also be called pressure sores or bed sores. They’re areas of damaged skin, and the tissue underneath the skin.
Pressure sores are caused by pressure or rubbing on the skin. They often happen when a client has difficulty moving, because the weight of their body puts pressure on certain areas. They are particularly common in clients who need to stay in bed or are unable to reposition themselves in their wheelchair.
They usually develop on bony parts of the body, such as the tailbone (just above the buttocks), heels, hips, or elbows.
Symptoms of pressure ulcers may include:
- discoloured skin
- a hard or spongy patch of skin
- pain in the affected area
- itching in the affected area
- blistering, in more advanced pressure ulcers
- open wounds, in more advanced pressure ulcers
When pressure sores are not treated, they can get worse, reaching deeper into the skin and muscles.
Untreated pressure sores can lead to cellulitis (skin and soft tissue infections) and osteomyelitis (bone infections), and even sepsis. Sometimes a pressure ulcer can develop into a Marjolin ulcer, a rare and aggressive cancer that forms in wounds or inflamed areas.
Pressure ulcers and their complications can be painful, and may lead to hospitalisation. Using a Waterlow Scale calculator can help you identify clients most at risk of pressure sores, and help prevent them from forming.
What should I do if a client has a pressure ulcer?
If you notice that a client has a pressure ulcer, document it. Use photographs or measurements where possible, so that you can check whether it is healing as expected.
You should also contact their GP or healthcare team.
To look after someone with a pressure ulcer, there are a few things you can do, including:
- Moving your client regularly, to reduce pressure on the site and stop new pressure sores forming
- Using specialised mattresses and cushions to keep your client comfortable
- Dressing the ulcer and changing dressings regularly
- Cleaning the ulcer if necessary
- Encouraging them to eat a balanced diet
- Supporting them to take any antibiotics or medication as prescribed
Do not use gauze dressings or topical antiseptics to treat pressure sores.
If your client’s pressure ulcer is persistent, it may need to be cleaned and closed in surgery.
If your client is in pain, has very hot or red skin around the pressure ulcer, a high temperature, or has pus coming from the pressure ulcer, call for medical help immediately. These could be signs of an infected pressure sore.

How to calculate Waterlow Score
Now that you know what the Waterlow Score is and what it’s used for, let’s talk about how to calculate Waterlow Score for a client.
Your organisation may have a Waterlow Score chart printable or hard copies already available, but if not, you can easily track and calculate scores using modern home care software.
Waterlow Score calculator
For each of the factors below, select the appropriate answer. You may need to choose more than one score in some categories.
Sex
- Male – 1
- Female – 2
Age
- 14-49 – 1
- 50-64 – 2
- 65-74 – 3
- 75-80 – 4
- 80+ –5
BMI
- Average (20-24.9) – 0
- Above average (25-29.9) – 1
- Obese (above 30) – 2
- Underweight (below 20) – 3
Skin condition
- Healthy – 0
- Dry – 1
- Tissue paper – 1
- Oedematous – 1
- Clammy – 1
- Painful over bony areas – 2
- Discoloured – 2
- Broken – 3
Continence
- Complete continence – 0
- Catheterized – 0
- Urinary incontinence – 1
- Faecal incontinence – 2
- Urinary and faecal incontinence – 3
Mobility
- Fully mobile – 0
- Restless or fidgety – 1
- Apathetic – 2
- Restricted – 3
- Fully bedbound – 4
- Fully chairbound – 5
Nutrition
- No recent weight loss and normal appetite – 0
- Recently lost 0.5-5kg or is eating poorly – 1
- Recently lost 5-10kg or is unsure of exact weight loss – 2
- Recently lost 10-15kg – 3
- Recently lost over 15kg – 4
Additional factors
- Previous history of pressure ulcers – 5
- Smoker – 1
- Medication such as steroids, beta blockers, or cytotoxics – 4
- Anaemia – 2
- Diabetes, well-controlled – 4
- Diabetes, poorly-controlled – 6
- Peripheral vascular disease – 5
- Multiple sclerosis – 4-6, depending on condition
- Reduced cognition – 4-6, depending on condition
- Paraplegia – 4-6, depending on condition
- Single organ failure – 5
- Multiple organ failure – 8
- Orthopaedic or spinal surgery in the last 48 hours – 5
- Surgery of longer than two hours in the last 48 hours – 5
- Surgery of longer than six hours in the last 48 hours – 8
- Terminal cachexia – 8
Now add up the scores in each category.
Waterlow Score meanings:
- 0-9 – not at risk
- 10-14 – at risk
- 15-19 – high risk
- 20 or higher – very high risk

Waterlow Score chart: the next steps
Once you’ve calculated your client’s Waterlow Score, you can take action.
If your client has a low Waterlow Score, meaning they’re not at risk of pressure ulcers, you don’t need to do anything. Instead, you should re-evaluate them regularly, especially after surgery, illness, or if they become less mobile.
However, if your client has a higher result on the Waterlow Score chart, meaning they’re at risk of pressure ulcers, you may need to make changes to their care plan within your care planning software.
How to prevent pressure ulcers
If your client is at risk of pressure sores, there are a few ways that you can help prevent them.
- Encourage your client to move regularly, or help them reposition themselves. This should happen every six hours for people at risk of developing pressure ulcers, or every four hours if their risk is very high.
- Use a specialist foam mattress or wheelchair cushion for clients who are at risk. Specialist pressure redistributing devices can help to reduce the stress on certain areas of the body.
- Use a barrier cream to improve your client’s skin health. If your client has very dry skin or other dermatological issues, tackling these problems can reduce their risk of developing pressure sores.
- Work with your client’s GP and other healthcare teams to treat any underlying health concerns. Some conditions, such as anaemia and poorly-controlled diabetes, can increase the risk of pressure ulcers.
- Encourage your client to stop smoking. Smoking is a risk factor for pressure ulcers, as it can impact circulation and delay wound healing.
- Educate your client, their family and other carers about the signs of pressure ulcers. Pressure sores may develop over days or in just a few hours, but identifying them and treating them quickly can reduce the chance of complications and hospitalisation.
You should not offer massage to prevent pressure sores, and there is no need to offer supplements if your client’s nutrition is good.
Conclusion: what is the Waterlow Score and what is it used for?
The Waterlow Score is a vital tool for health and social care professionals, allowing you to assess a client’s likelihood of developing pressure ulcers.
Integrated with reliable care management software, it looks at a range of factors, including mobility, BMI, continence, and underlying health conditions.
Carers and other healthcare workers should learn how to calculate Waterlow Score for a service user, and reassess them regularly. Identifying which clients are most at risk allows you to take preventative action, meaning that you can keep them comfortable, safe, and healthy.