Heatwaves are becoming more common across the UK, and while sunshine can be enjoyable, high temperatures present serious risks for home carers and the vulnerable clients they support.
Issues such as heat stress, dehydration, and fatigue can quickly escalate, leading to significant health consequences.
In this guide, we’ll cover five practical and proven strategies to keep your carers and clients safe and comfortable during the hottest days of summer.
Table of Contents
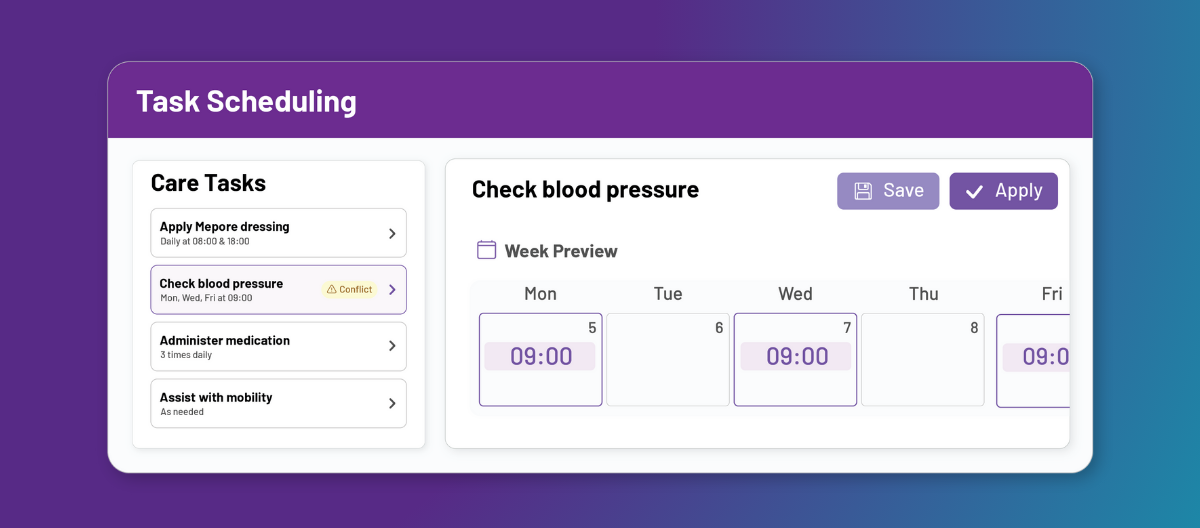
1. Schedule high-risk visits during cooler hours
Activities scheduled during the hottest part of the day (typically between 11am and 3pm) significantly increase the risk of heat-related illnesses. The NHS specifically recommends limiting outdoor activities during these peak heat hours.
What you can do:
Adjust staff rotas so outdoor visits, shopping trips, or physical activities occur during cooler morning or evening hours. Encouraging clients to remain indoors during peak heat helps reduce risk and discomfort.
2. Provide regular hydration breaks for carers
Dehydration not only impacts physical performance but also affects concentration and decision-making. The Health and Safety Executive (HSE) emphasises the importance of regular hydration to prevent heat stress in the workplace.
What you can do:
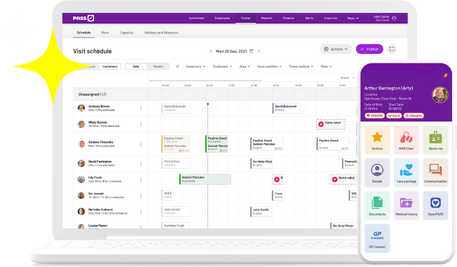
Build mandatory hydration breaks into carers’ schedules, especially during hot weather. Ensure carers carry water with them at all times and encourage regular drinking. Reminders through your care management software or team meetings reinforce good hydration practices.
3. Use heat-safety checklists
Simple, preventive steps can often be overlooked during busy shifts. Following structured checklists ensures carers consistently implement essential safety measures during heatwaves.
What you can do:
Provide carers with clear, actionable heat-safety checklists covering room ventilation, client hydration monitoring, and recognising early symptoms of heat stress.
The official Heatwave Plan for England by Public Health England offers detailed, evidence-based guidance to build your checklist. Using digital checklists in care planning software can help ensure compliance and quick reporting.
4. Closely monitor vulnerable clients
Some clients are particularly vulnerable during heatwaves, including those with chronic health conditions, elderly clients, and individuals with limited mobility. The NHS identifies these groups as high-risk during periods of extreme heat.
What you can do:
Create and maintain a priority list of high-risk clients. During heatwaves, closely monitor their care notes for early signs of heat-related illness, such as confusion, dizziness, or changes in behaviour.
Early intervention can prevent serious complications. Digital alerts or risk tracking within dedicated home care software can significantly streamline this process.
5. Encourage proactive communication about heat risks
Carers are on the frontline and often the first to spot potential problems, but they may hesitate to speak up if communication channels aren’t clearly supportive and open. The HSE Talking Toolkit highlights how proactive communication enhances workplace safety.
What you can do:
Regularly remind carers to promptly report any heat-related concerns or incidents. Cultivate a culture where safety concerns are actively encouraged and quickly acted upon without fear of judgment or blame.
Conclusion
Proactive planning and effective communication are essential to safely managing heatwaves in home care. By implementing these five practical strategies, you can protect the wellbeing of your carers and clients, keeping everyone safe and comfortable even when temperatures soar.
Stay cool, stay safe, and stay prepared!