As a care professional, you’ll need to help your clients take medication. And when you do that, you should use a MAR chart.
Many of your clients will take multiple types of medication each day. Some will be prescribed by a doctor, and others might be over-the-counter drugs or alternative remedies. And, for clients with complex health needs, memory difficulties, or mobility issues, you may need to administer this medication for them.
A MAR chart records when a carer has administered medication to a service user. Each time the client receives a dose of medication, the chart should be signed.
In this article, we’ll look at what a MAR chart is, when you should use one and how, where you can find MAR chart templates, and some of the most common mistakes in medication administration.

Table of Contents
What is a MAR chart?
A MAR chart is a record of medication administered to a client. It should contain information about prescription and over-the-counter medication that a service user needs.
A MAR chart should include:
- The client’s name and date of birth
- The client’s GP
- The medication name, formulation and strength
- How often or when the medication should be taken
- How the medication should be administered – sometimes known as the route of administration
- Any additional notes about the medication – for example, should it be taken after eating, or on an empty stomach?
- A stop or review date for the medication, if applicable
- Details of any reactions or allergies to medication or ingredients the client may have
- What support the client needs to take medication
MAR charts are an important part of keeping clients safe. Medication errors can cost lives. Reading a MAR chart each time you administer medication reduces the chance of making mistakes – and also means that, if an error does happen, care staff can notice it quickly and take action.
MAR sheets help to keep your clients safe, but they can also protect you. In the event of an inquiry or investigation, accurate record-keeping is important. These records may be used as evidence in investigations or court cases, so it’s crucial to make sure that a MAR chart for domiciliary care or care home clients is clear, accurate, and up-to-date.
A MAR chart is a legal requirement under the Health and Social Care Act 2008.

What does MAR chart stand for?
MAR stands for Medication Administration Record.
Some organisations may also use the term kardex. If your organisation uses care management software for their MAR charts, you may also hear them called eMAR systems or electronic MAR charts.
When should I use a MAR chart?
As a care worker, there are several ways that you might help a client with their medication, including:
- reminding them to take their medication
- helping them to remove medication from packaging or other preparation
- administering the medication for them
Every time you do one of these activities, you should use a MAR chart.
If a family member or friend helps the client with medication, they should also sign the MAR sheet when they do so.
If a service user is entirely responsible for their own medication, you do not need to use a MAR chart. For example, if you only support a client with bathing and housekeeping, a MAR sheet isn’t necessary, even if they take medication themselves.

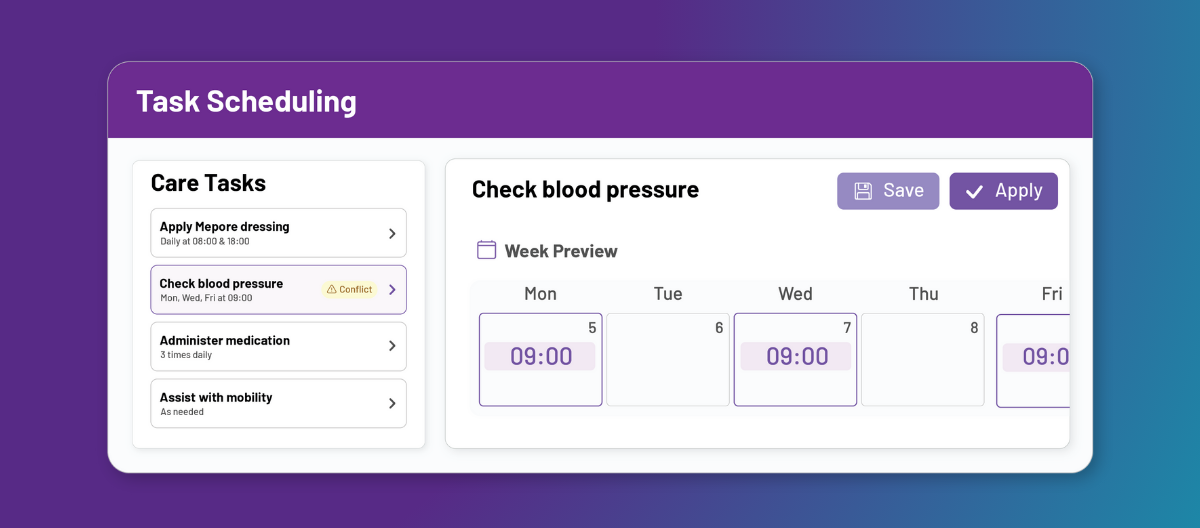
Manage medication safely with PASS 💊
PASS includes a built-in eMAR, giving your team a clear, digital record of every dose. Real-time updates, reminders, and audit trails reduce errors and make HIQA compliance easier.
Book a tour today to see how PASS can support your organisation in delivering safer, smarter medication management.
Which medication should be recorded on a MAR chart?
MAR charts should include all medication. This includes:
- Prescribed medication
- Over-the-counter medication
- Alternative or home remedies
You should include all medications, whether they’re taken in pill or liquid form, injected, applied as a cream, gel or patch, or any other method.
Service users may take some medication regularly – for example, blood pressure medication that must be taken daily. However, some medication is only given occasionally, when required – such as painkillers or anti-nausea drugs. This should also be included on a MAR sheet.
Having an accurate record of all medication taken reduces the risk of medication errors, as well as dangerous interactions between drugs.

How do you complete a MAR chart?
All care workers at your organisation should learn how to fill in a MAR sheet, if they support clients to take medication. This should be part of your training for carers. As part of your training, your supervisor will probably show you a MAR chart example, so you know what a filled-in MAR sheet looks like. If you use an eMAR system, you should be trained on this too.
Depending on your organisation’s systems, the process of completing a MAR sheet might be slightly different. But, in most cases, you’ll do the following:
- At the start of a new MAR sheet, fill in the details required. This will probably include your client’s full name, date of birth, GP, and known allergies or reactions.
- Record the details of your client’s medication, checking the details against the pharmacist’s label. Take special care when recording details of dosages, such as mcg (microgram) and mg (milligram). Include details about when and how often the medication should be taken.
- Support your client to take their medication. Do not sign the MAR chart before your client has taken the medication.
- After you have administered the medication, or helped the client take their own medication, sign or initial the correct box on the MAR sheet. Enter the time and date.
- If the medication is to be given only as needed (PRN), you may need to note why it was required.
- If the medication is not taken, note why.
If you use paper MAR sheets, write in ink. Avoid using pencil, and don’t use correction fluid on a MAR chart.
MAR chart codes
MAR sheet codes help care workers note down common medications, dosage information and situations quickly, using a minimum of space. Some of these abbreviations will be written on your client’s medication packaging, and you may need to use others when completing a MAR chart.
If you don’t understand MAR chart codes or abbreviations, ask a supervisor. Don’t make assumptions about a service user’s medication – errors can be fatal.
Meaning of MAR chart codes:
- Dosage:
- gt or gtt: drops
- i: one tablet
- ii: two tablets
- iii: three tablets
- mg: milligrams
- mcg: micrograms
- ml: millilitres
- Route of administration: these codes describe how a medication should be taken or administered
- PO: orally
- PR: rectally
- IM: intramuscular
- SC: subcutaneous
- TOP: topical
- Time of administration: not all medications will need this instruction, and some may simply say how often they should be taken
- AM: morning
- PM: afternoon
- AC: before meals
- Frequency of administration: this describes how often the medication is needed
- QH: hourly
- BID or BDS: twice daily
- QDS: 4 times a day
- OD or QD: once daily
- QOD: every other day
- Q 1 h: every 1 hour (different numbers may be substituted)
- Q 1 d: every 1 day (different numbers may be substituted)
- PRN: as required
- To be completed after the medication has been administered:
- T: taken
- R: refused
- E: refused and destroyed
- NT: not taken, if the client was not available at the time
- NR: not required
- P: prompted
- M: made available
- ADM: administered by
- WT: witnessed by
If your organisation uses any specialised MAR chart codes, these should be explained to you during your training.

Where can I get a MAR chart template?
Many care organisations use pre-printed MAR charts from the pharmacy. These may be delivered with the medication. The pharmacy MAR sheets usually cover a period of 28 days, and you might use a separate one for each medication.
Alternatively, your organisation may produce their own MAR chart templates that you can print or photocopy.
Advantages of paper MAR chart templates:
- Cheaper to set up
- MAR sheets can be kept with the medication
- Very little training required
- No need to worry about power cuts or system malfunctions
However, there are some disadvantages to paper MAR sheets. For example, it might be hard to read a care worker’s handwriting, and sometimes carers might not fill the sheet in completely. You also need to have a safe storage place, as you should keep MAR sheets for at least eight years after your care service has stopped supporting the client. And, of course, paper charts are less secure than a password-protected electronic system.
The alternative to paper MAR chart templates is an eMAR system. If your organisation uses care management software, this may already include an eMAR system.
Advantages of eMAR systems:
- Can be accessed anywhere, as long as you have care management software installed on your phone, tablet, or computer
- Secure, and reduces the risks of losing physical paperwork
- Entries are stamped with the carer’s details, as well as the time and the date, making it quicker to complete
- Can provide medication alerts and reminders
- Multiple care team members can have access to the online system
- No need to worry about decoding messy handwriting
- No need to worry about physical storage


Common MAR chart mistakes and how to avoid them
MAR charts are helpful tools for medication safety, but care workers are still human – and we all make mistakes occasionally. Let’s look at some of the most common MAR sheet errors, and how you can avoid them.
If you’ve made a medication error, call for help immediately.
Some of the most common mistakes include:
- Failing to include allergies, reactions, or other relevant medical history. If a client can’t communicate or remember their own details, it’s essential to liaise with their GP or family to complete a full medical history.
- Using non-standard MAR chart codes. It might seem intuitive to make up your own abbreviations, but others may not understand them. Remember that you’re not only recording this for yourself – a MAR chart could become evidence in investigations or audits.
- Pre-charting. When you’re working quickly, you may want to complete the record before your client has taken their medication. However, you should wait until the medication has been taken, so that you can accurately record whether it was administered successfully.
- Not including the time and date of each medication administration. If you’re in a hurry, it can be tempting to simply sign your name and plan to add the date and time later – but you should complete the MAR sheet fully at the time.
Using electronic records, such as the PASS eMAR system, can help you record medication administration quickly and accurately, and avoid making these mistakes. Many providers now use home care software with built-in eMAR tools, helping teams administer medication safely and reduce errors.
The eMAR system can remind care workers to give medication and fill out the record. Carer details, times and dates are tied to each entry, so it’s quicker to use an eMAR system – reducing the risk of mistakes made in a hurry.
Not only that, but GP Connect can help you access a service user’s medical history, so that you can easily fill out the basics of a MAR sheet.
If your care team are regularly making mistakes with MAR charts, consider whether your training and onboarding systems are working. Remember, MAR chart errors can be fatal.
Conclusion: MAR charts for domiciliary care and care homes
Providing great care is something all support workers strive for, and MAR charts can help them with that.
Some organisations use paper MAR sheets, and others use eMAR systems. Whether you work in a care facility or support clients in their own homes, keeping records of medication administration is a legal requirement. Not only does it help to keep your clients safe, it can protect you as well.
Digital tools like care planning software make this easier by linking MAR charts directly with care notes and risk assessments, giving managers a full picture of each client’s health.