Eating well is important for all of us, but the importance of nutrition for elderly people can’t be overstated. As care providers, you’ll often be responsible for meal planning and food preparation for your clients, so it’s important to understand their needs.
Like getting enough sleep, nutrition is important for all of us, whatever our age. Making good food choices gives us the right amount of energy and helps us keep a healthy weight.
But for older people and those with certain health conditions, it’s even more important.
Many of your service users might have complex health conditions – which might have an impact on the food they should eat.
Whether you provide domiciliary care or work in a care facility, you should work with your clients, their families, and their medical teams to come up with a healthy and safe meal plan for them.
Home care software can support care teams in tracking dietary needs and ensuring clients receive the right meals based on their individual health conditions.
In this guide, we’ll look at the dietary requirements for elderly people, the importance of nutrition for people with complex health conditions, and, of course, hydration for seniors.
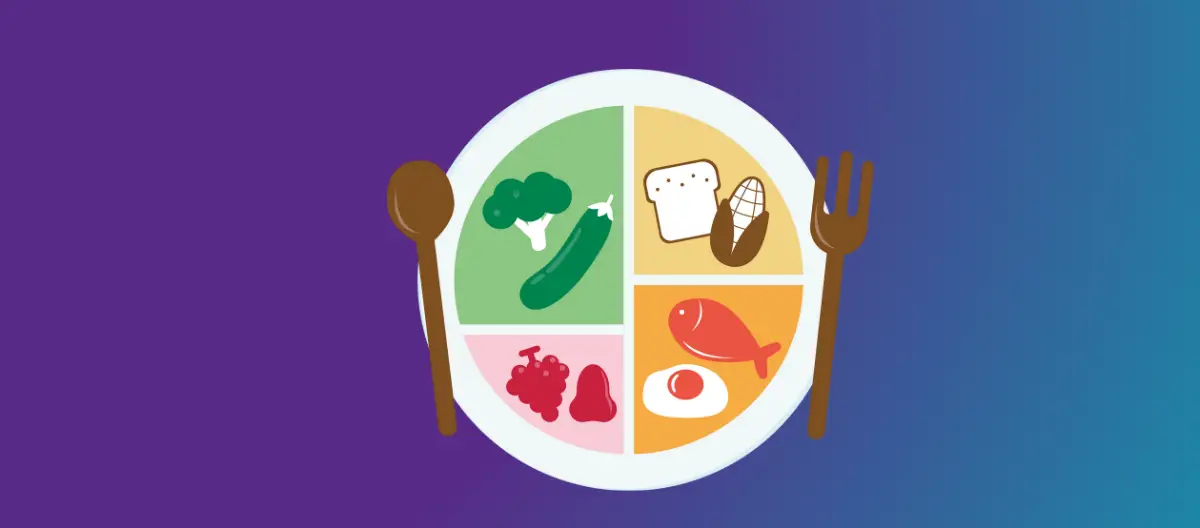
Table of Contents
Why do elderly people eat less?
Lots of older people eat less than they did when they were younger. There can be a few reasons for this, including:
- Having a lower appetite due to being less active
- The loss of a partner or family member who used to prepare food
- Finding it harder to prepare food for themselves, often due to mobility difficulties
- Depression or low mood leading to a low appetite
- Tooth pain or loss causing difficulty chewing
- Problems with swallowing, sometimes caused by a stroke or other medical event
- Having new dietary restrictions, and struggling to feel excited about food
But not all older people want to eat less. So if you’re preparing healthy food for seniors as part of your caring role, make sure that you check with them about their dietary needs. Some older people, especially if they’re still very active, may still want and need a larger meal.

Dietary requirements for elderly people
In most cases, older people should eat a balanced diet over the course of a day or week, just like younger people. The NHS Eatwell Guide provides advice on what we should all work towards, and dietary requirements for elderly people are often the same as for the younger population.
A balanced diet should include:
- At least 5 portions of fruit or vegetables each day – this can include fresh, frozen, tinned, dried, or juice and smoothies.
- Starchy food, which should account for around a third of the food we eat. This includes bread, potatoes, pasta and rice.
- Foods high in protein, such as meat or fish, eggs, beans and pulses.
- Foods high in calcium, such as dairy or alternatives.
- Foods high in fibre, such as whole grains, pulses, vegetables and fruit.
Very sugary and salty foods, such as chocolate, crisps, and cakes, don’t provide great nutrition for the elderly, and should be eaten in moderation – they shouldn’t be the main part of anyone’s diet.
Importance of nutrition for elderly people with complex health conditions
Depending on their personal circumstances, your clients may have different dietary requirements.
As part of the care planning process, you should discuss the client’s health conditions and any dietary needs. You may need to involve other members of their healthcare team in these discussions.
While we can’t explore every possible diet in this article, you may need to prepare:
- A pureed or soft diet for elderly people
- A low sodium (or low salt) diet
- Meals for people living with diabetes
- Meals for people living with dementia
- Food for people with allergies or intolerances
Soft diet for elderly people
Some service users may need a soft or pureed diet. This might be because they have difficulty chewing or swallowing. Pureed food is smooth and doesn’t need to be bitten or chewed, so there is less of a risk of choking.
You may need to use a blender or food processor to puree food for your clients, or mash it by hand. You should use a sieve to remove any remaining small pieces that could be a choking risk.
Tips for creating a pureed meal:
- Blend and puree each part of the meal separately, so that it looks more appetising and keeps its individual flavour.
- Add milk, cream, or gravy to make the food easier to blend.
- Use a mould or piping bag to shape the food in an attractive way for your clients.
- Pureed food should be able to hold its shape on a fork or spoon – if it’s too watery, add flour or another thickener.
If your clients need a soft diet, make sure that they avoid chewy food, like dried fruits, and food with skins, such as grapes.

Low sodium diet
It’s usually a good idea for older people to eat less salt, but some clients may have been told to restrict their salt intake by their healthcare team. This might be because they already have high blood pressure.
Salt can increase our blood pressure, and high blood pressure increases the risk of stroke and heart failure. Salt might also increase the risk of developing osteoporosis (brittle bones).
If you’re supporting someone who needs a low sodium diet, you may need to prepare lots of food from scratch. Many ready-made meals contain high amounts of salt.
Tips for supporting someone with a low sodium diet:
- Don’t add extra salt to meals while you’re cooking or at the table.
- Provide other seasoning options for your clients.
- Make meals from scratch, and avoid buying too many pre-prepared meals and food items. Even shop-bought bread and soups are likely to be quite high in salt compared to homemade versions.
- If you need to use ready meals or pre-prepared snacks, look for ones that say they’re low in salt.
Meals for people living with diabetes
If your client has diabetes, they may have some additional dietary requirements. This may include counting carbs, eating a lower-calorie diet, cutting down on sugar, or eating more fruit and vegetables.
They may also need to take medication and check their blood sugar regularly.
There are several different types of diabetes, and everyone’s condition is different. Keep talking to your client about how they’re feeling, and encourage them to check in with their diabetes team if they have questions about how they should be eating.
Meals for people living with dementia
If you’re supporting a client with dementia, you might notice that they develop additional challenges with eating and drinking as their condition progresses.
Some people with dementia may not recognise the signs of feeling hungry and thirsty, or may struggle with remembering how to feed themselves. Their food preferences may change, and some people may struggle to communicate their feelings about a meal.
Tips for preparing food for people with dementia:
- Prepare and offer small meals, especially if larger meals go uneaten. You can always prepare more later on.
- Offer feeding help if your client struggles to feed themselves.
- If your client can’t focus on an entire meal, provide healthy snacks and smaller meals that can be eaten on the go.
- Offer finger foods rather than meals that need to be eaten with cutlery.
- Make sure that your client doesn’t have any mouth pain and that any dentures are properly fitted.

Food for people with allergies or intolerances
Food allergies and intolerances can be severe. If a client has a food allergy, discuss how it usually presents and how it should be treated.
Some allergies are very well-known, such as nut allergies or lactose intolerance. Others are less common, and can be harder to manage. There are 14 major allergens that should be mentioned on all food packaging – but your service users may have other allergies or intolerances.
Some people only react to the food if they eat it. Others might have a reaction if their food was prepared using utensils that touched their allergen, and others may react just by being in the same room as the allergen.
Allergic reactions may include developing a rash, being sick or having diarrhoea, or feeling dizzy.
Some people may have an anaphylactic reaction, where their throat, mouth or tongue swells up, they find it difficult to breathe, they suddenly faint, or their skin or lips turn blue or grey. This is a medical emergency, and you should call 999 immediately.
Tips for supporting a client with a food allergy:
- Make sure that the catering team and any care staff are aware of the client’s allergy.
- Read the ingredients on all pre-prepared food – even if it’s usually safe. Catering companies may change recipes without warning.
- Be aware of the dangers of cross-contamination. You may need to prepare food in a separate area, or use different utensils, cookware, and appliances such as toasters.
- Make sure that the care team are aware of the signs of exposure, and how to help the client.
- If your client needs an Epi-Pen or other allergy medication, make sure that it’s with them at all times, and that the care team are aware of how to use it. Use eMAR software to record when it has been used and keep track of any concerns.
Planning and preparing healthy food for seniors
We’ve talked about dietary requirements for elderly people, and how to accommodate different diets for health-related reasons.
Just like the rest of us, though, older people will have food preferences and other dietary restrictions. Some of your clients may be vegan or vegetarian, keep kosher, follow a halal diet, or have strong likes and dislikes.
As part of the care planning process, you should discuss the client’s health conditions and any dietary needs. Using a reliable care management software can help ensure dietary preferences, allergies, and nutritional requirements are well-documented and easily accessible for the care team.
If you work in a care home with set meal times and menus, this might be a difficult adjustment for new clients. If possible, see if you can talk to the catering team about accommodating individual preferences, or preparing varied healthy snacks for service users to have at other times.
Hydration for seniors
Fluid intake for older adults is important. If your client doesn’t drink enough, they increase their risk of developing urinary tract infections, kidney stones, cognitive impairment, or even seizures.
How to spot the signs of dehydration:
- Urinating less often
- Dark or strong-smelling urine
- Feeling dizzy or faint
- Feeling tired
- A dry mouth
- Sunken eyes

Most older people need to drink around 6-8 glasses of fluids a day. It’s okay if this is water, diluted squash, milk, or tea or coffee. They may need to drink more if they’ve been very active and sweating, have a high temperature, have been sick or have diarrhoea, or have been in a warm environment.
If your service users have mobility difficulties or dementia, or are taking medication that makes them feel drowsy or unwell, they may find it harder to stay hydrated.
Tips to help your clients stay hydrated:
- Make sure they always have a drink within reach.
- Offer a variety of drinks, such as water, squash, tea and coffee.
- Try different cups, glasses or bottles. Some clients may prefer to drink from a straw.
- Sit with them and have a cup of tea yourself.
- Provide foods with high water content, such as watermelon and soup.
Conclusion: Nutrition for the elderly
Why is nutrition important for the elderly? Like all of us, older people need to have the energy for their daily activities, and keep a healthy weight. However, many older people have additional health concerns, which have an impact on the food they should eat.
As a care provider, you should work with your clients, their families, and their healthcare teams, to ensure that you’re preparing food that can help them stay healthy and independent for as long as possible.